Acute musculoskeletal injuries and chronic musculoskeletal disorders often result from participation in high-demand activities, particularly during sports. These conditions lead to pathological changes in the soft tissues that enable skeletal movement, such as the muscles, tendons, ligaments, and cartilage, and ultimately, alterations in forward movement. Such modified gait patterns may arise from inherent tissue-level adaptations that occur soon after injury and surgical intervention. Current clinical assessments have a limited scope and are unable to objectively classify both post-surgery tissue status and to quantify active patient function. As a result, specific relationships between in vivo soft tissue properties and altered movement patterns remain unclarified in many high-incidence injury models.
With this in mind, the aims of this subgroup are to objectively assess both (1) changes in musculoskeletal tissue properties instigated by injury and disease and (2) the adaptive changes in lower extremity movement that coincide with these altered tissue properties. The central goal is to develop a comprehensive understanding of the relationship between these two aspects to improve clinical outcomes.
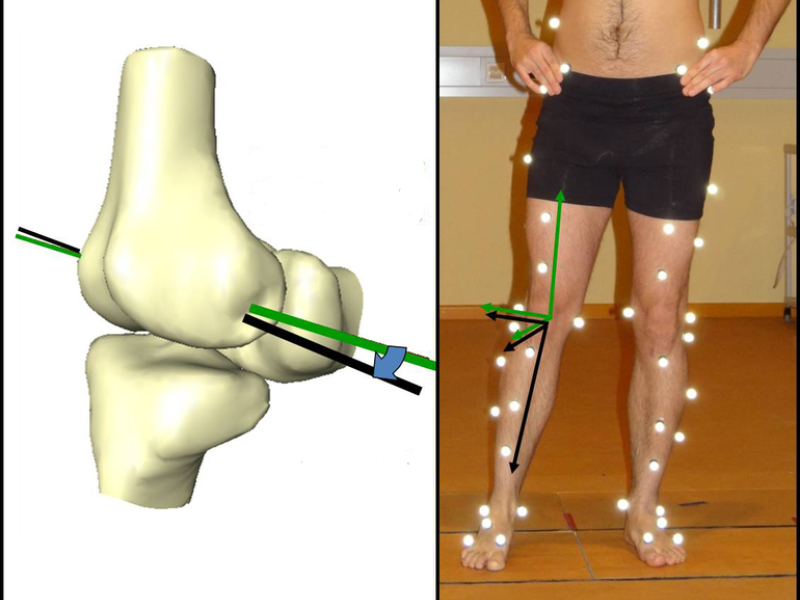
In order to achieve this, both pre-existing and newly developed methods have been employed to monitor tissue function. Sample projects include fluoroscopic assessment of the knee during both passive and active movements. Furthermore, we have developed validated kinematic methods and algorithms in order to more accurately determine joint centers and axes to monitor in vivo skeletal movement during motion analysis. Applications of the OCST method developed within this cooperation for significant reductions in soft tissue artefacts. Finally, various types of functional assessments in the lower limb have been cross-checked and compared, e.g. active versus passive, single-limb and bilateral assessments. These types of assessments are particularly interesting with the context of sports-related injuries that typically occur unilaterally, such as anterior/posterior cruciate ligament (ACL/PCL) or Achilles tendon ruptures and reconstructions.